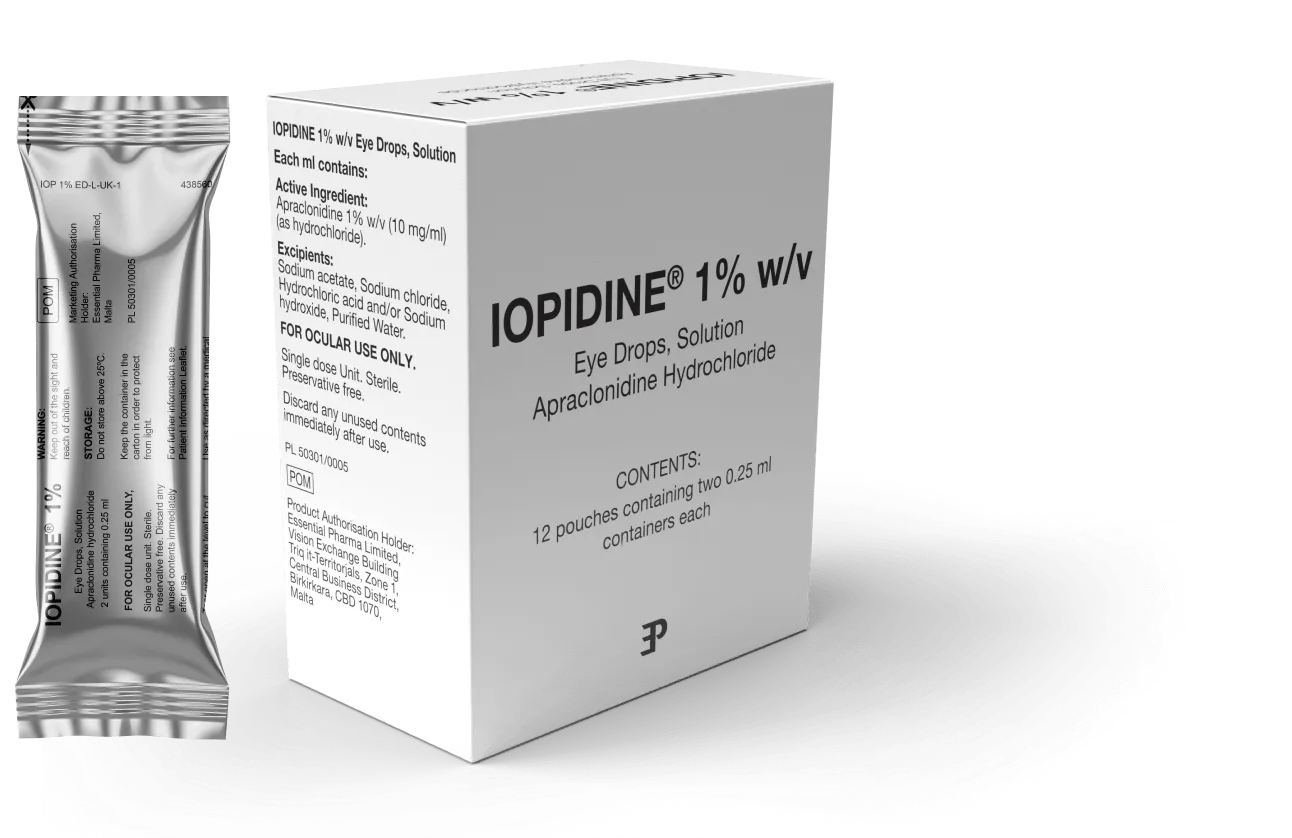
IOPIDINE® 1% w/v
Apraclonidine hydrochloride 10 mg/ml eye drops, solution
Intraocular pressure (IOP) spikes after anterior segment laser procedures are common, difficult to predict and can result in damage in optic nerves and visual acuity loss.1
Spikes usually occur within 3 hours of laser procedures,1 so the use of medications to lower IOP and prevent post-surgical spikes is recommended.2,3 IOPIDINE® 1% is indicated for the control or prevention of post-surgical elevations in intraocular pressure that occur in patients after anterior segment laser surgery. (Clinical trials have been conducted in trabeculoplasty, iridotomy and capsulotomy).4
What is apraclonidine?
Apraclonidine is a potent and relatively selective α2-adrenergic receptor agonist.1 Several studies show that apraclonidine lowers IOP by decreasing aqueous production through its action on α2-adrenoreceptors of the nonpigmented ciliary epithelium.1
In January 2022 NICE revised the guidelines for the management of raised intraocular pressure, laser surgery is now recommended as first line treatment ahead of topical medication.3
The European Glaucoma Society (EGS) guidelines recommend the use of medications including α2-adrenergic receptor agonists before and immediately after laser surgery to prevent IOP spike, including apraclondine.2
Benefits of IOPIDINE® 1%
IOPIDINE® 1% is a proven and efficacious way to control intra-ocular pressure after laser surgery.
IOPIDINE® 1% has been shown to prevent and control post-surgical elevations in intraocular pressure, lowering and demising the frequency of IOP spike.5
Treatment with IOPIDINE® 1% resulted in statistically significant reductions in IOP versus placebo up to 3 hours after the operation.5
Mean IOP of eyes treated with IOPIDINE® 1% (n=39) and placebo (n=34) after argon laser trabeculoplasty.5
Adapted from Robin AL et al Arch Ophthalmol. 1987;105:646–650
NS; Non-significant
Axis has been split for restricted space
In patients with narrow angle glaucoma treated with argon laser iridotomy, 43% of the eyes treated with placebo, and none of the IOPIDINE® 1% treated eyes, experienced an IOP rise greater than 10mmHg above baseline within the first three hours.6
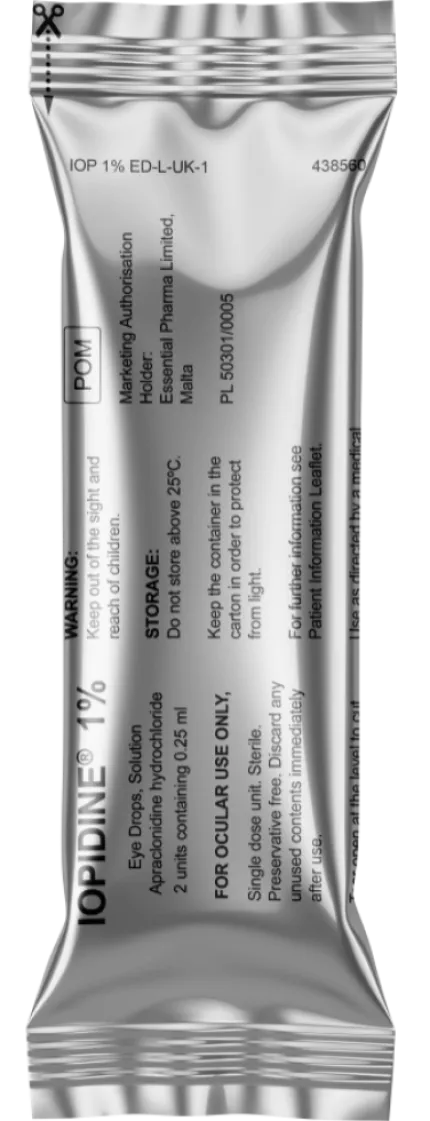
IOPIDINE® 1% is available as a unit dose preservative-free treatment.7
Additional benefits of IOPIDINE® 1%
IOPIDINE® lowers IOP with minimal CNS side effects.1 Based on a real-world study, use of topical apraclonidine showed to have no significant effect on blood pressure and heart rate.8†
IOPIDINE® 1% is available as a unit dose preservative-free treatment7 to prevent raised IOP after anterior segment laser surgery.4 It is easily administered as one drop one hour before anterior segment laser surgery, and one drop immediately after the procedure.
†Study investigating IOP elevations after anterior segment laser surgery (n=66).

Safety information
IOPIDINE® is contraindicated in patients with a history of severe or unstable and uncontrolled cardiovascular disease.3
IOPIDINE® 1% is contraindicated for use in children.4
IOPIDINE® 1% is contraindicated in patients receiving monoamine oxidase inhibitor therapy, systemic sympathomimetic agents and tricyclic antidepressants.4
IOPIDINE® 1% is contraindicated in patients with hypersensitivity to the active substances (clonidine or apraclonidine) or to any of the excipients.4
In clinical trials, common adverse events included dry mouth (5.6% of patients), eyelid retraction and mydriasis (approximately 3% to 4% of patients). All other drug reactions occurred in fewer than 2% of patients.4

